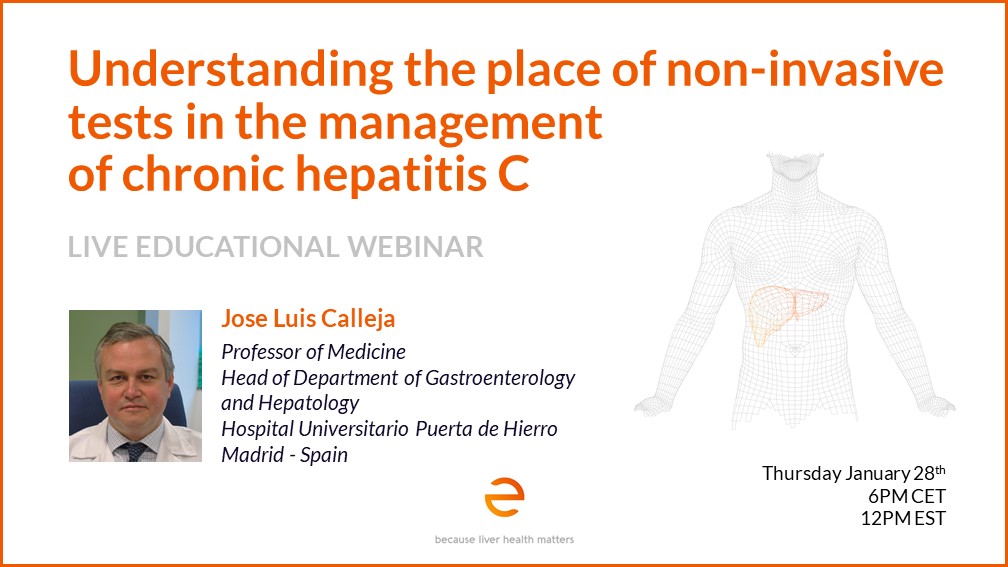
About Prof. Jose Luis Calleja
Jose Luis Calleja is the head of the Gastroenterology and Hepatology Department at the Hospital Universitario Puerta de Hierro and is Professor of Medicine at the Universidad Autonoma de Madrid in Madrid, Spain. He received his Medical Degree and Doctorate from the Universidad Autonoma de Madrid. Prof. Calleja is the main author of several national and international publications in gastroenterology and hepatology. He has been a principal investigator on several research projects and multicentric international clinical trials. He has been the principal investigator of different projects in viral Hepatitis, cirrhoris and NASH. He is Vicepresident and Elect President of the Spanish Association for the study of the liver (AEEH).
Understanding the Place of Non-Invasive Testing in the Management of Chronic Hepatitis C
The advent of safe, well-tolerated, and highly efficacious direct-acting antiviral (DAA) therapy for chronic HCV infection has revolutionized care and makes elimination of hepatitis C conceivable. However, multiple efforts are still needed to achieve this ambitious goal set by WHO in 2016.
During this webinar, we will discuss the potential role of non-invasive tests and of FibroScan®, which when used in efficient case finding strategies, can help better test, diagnose and treat the remaining infected patients.