SSM@100Hz by FibroScan® Improves the Non-Invasive Diagnosis of CSPH, Supporting its Implementation into Clinical Practice

Study reference
Jachs, et al. Spleen stiffness measurement by vibration-controlled transient elastography at 100 Hz for non-invasive predicted diagnosis of clinically significant portal hypertension in patients with compensated advanced chronic liver disease: a modelling study. The Lancet 2024
| Population type | Compensated Advanced Chronic Liver Disease (cACLD) due to MASLD (40%), MetALD or ALD (33%), viral hepatitis (18%) or other chronic liver diseases (9%) |
| Sample Size | 407 patients with cACLD from 16 expert centers in Europe between Jan 1, 2020, and Dec 31, 2023 |
| Main objective | Assess the diagnostic utility of spleen stiffness measurement (SSM) at 100 Hz as a standalone non-invasive test for CSPH and to evaluate its incremental value compared with the ANTICIPATE±NASH model in patients with cACLD |
| Main Outcome | Clinically Significant Portal Hypertension (CSPH) |
| Acronyms | AUC: Area Under the Curve MASLD: Metabolic dysfunction Associated Steatotic Liver Disease MASH: Metabolic dysfunction Associated Steatohepatitis MetALD: Metabolic dysfunction-associated steatotic liver disease (MASLD) with increased alcohol intake ALD: Alcoholic Liver Disease cACLD: compensated Advanced Chronic Liver Disease CSPH: Clinically Significant Portal Hypertension SSM: Spleen Stiffness Measurement LSM: Liver Stiffness Measurement VCTE: Vibration-Controlled Transient Elastography HVPG: Hepatic Venous Pressure Gradient NICER Model: Non-Invasive CSPH Estimated Risk Model |
Background & objectives
Clinically significant portal hypertension (CSPH) is a serious complication of compensated advanced chronic liver disease (cACLD) that significantly increases the risk of morbidity and mortality.
The current gold standard for diagnosing CSPH is the invasive hepatic venous pressure gradient (HVPG) measurement, which is not widely accessible outside specialized centers.
To address this, the Baveno VII faculty recommended using non-invasive tests to estimate CSPH probability and guide the need for treatment with non-selective β-blockers such as carvedilol.
These tests, including the ANTICIPATE and subsequent ANTICIPATE-NASH models are based on liver stiffness measurement (LSM), platelet count and for obese MASH patients, BMI often face limitations due to diagnostic uncertainty in specific patient groups.
Recently, spleen stiffness measurement (SSM) using vibration-controlled transient elastography (VCTE™) at 100Hz has shown promise as a reliable and non-invasive alternative, especially when used in combination with other markers.
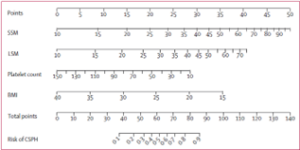
This study evaluated SSM by VCTE™ at 100 Hz as a standalone test, combined with platelet count and BMI, and as part of the comprehensive Non-Invasive CSPH Estimated Risk (NICER) model, which integrates SSM, LSM, platelet count, and BMI (see Fig. 1).
Figure 1. Nomogram of NICER model predicting CSPH in patients with compensated advanced chronic
Methods
A total of 407 patients with various chronic liver diseases and cACLD were recruited from 16 expert centers across Europe between January 1, 2020, and December 31, 2023.
The patients were divided into two groups: a derivation cohort (2020–2022) and a validation cohort (2023).
Each patient underwent a HVPG measurement, SSM by VCTE™ at 100 Hz, LSM by VCTE™ at 50 Hz, and platelet count testing. The HVPG measurement served as the reference standard for diagnosing clinically significant portal hypertension (CSPH), defined as HVPG ≥10 mmHg.
Results
Three models were evaluated in the study: SSM as a standalone test, LSM combined with platelet count and BMI (ie, ANTICIPATE-NASH), and a comprehensive model integrating SSM, LSM, platelet count, and BMI (NICER model).
SSM by VCTE™ at 100 Hz was shown to be a highly accurate non-invasive tool for diagnosing CSPH in patients cACLD.
Among the models, the NICER model outperformed the existing ANTICIPATE-NASH model, achieving superior diagnostic accuracy with an area under the curve (AUC) of approximately 0.9 in both derivation and validation cohorts (see Table 1).
| AUROC prediction of CSPH | Derivation cohort | Validation cohort |
| SSM | 0.779 | 0.830 |
| LSM | 0.718 | 0.804 |
| SSM, PLT, BMIH | 0.849 | 0.873 |
| ANTICIPATE +/- NASH | 0.849 | 0.863 |
| NICER model | 0.889 | 0.906 |
Table 1. Diagnostic performance measures of Baveno VII criteria and diagnostic algorithms considering SSM in derivation and validation cohorts
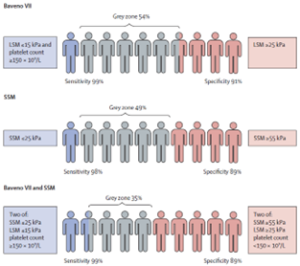
In the validation cohort, the Baveno VII criteria accurately ruled out CSPH, with high sensitivity (99.2%) for ruling out and high specificity (91.1%) for ruling in, although a significant number of patients remained in the diagnostic gray zone (54%).
The SSM cutoffs proposed by Baveno VII (21 kPa and 50 kPa) showed acceptable sensitivity but low specificity, which could be improved by adjusting the cutoffs to 25 kPa and 55 kPa, maintaining similar gray zones (see Fig. 2).
Figure 2. Performance of cutoffs for ruling in and ruling out clinically significant portal hypertension Baveno VII and SSM in the validation cohort
Take home messages
- Patients included in the study had MASLD (40%), MetALD or ALD (33%), viral hepatitis (18%), and other chronic liver diseases (9%), demonstrating the applicability of these diagnostic tools across various liver conditions.
- Adding SSM to LSM, BMI, and platelet count (NICER model) outperformed the ANTICIPATE±NASH model for CSPH risk stratification in cACLD patients, showing that SSM enhances the non-invasive diagnosis of CSPH and supports its adoption in clinical practice.
- SSM achieved a high success rate of approximately 94%, with its diagnostic performance unaffected by measurement variability (IQR).
- The Baveno VII criteria, which rely on LSM and platelet count, leads to a substantial proportion of patients being in the “gray” indeterminate zone. This can be reduced by incorporating SSM into sequential or combined algorithms with LSM and platelet count.
- The universal point-of-care risk stratification algorithm developed addressed the limitations of the Baveno VII criteria enabling application in patients with MASLD and obesity.
In this European multicenter study of patients with cACLD, predominantly due to metabolic diseases, SSM by VCTE™ at 100 Hz significantly improved non-invasive diagnosis of CSPH compared to standard methods. The comprehensive model (NICER) incorporating SSM, LSM, platelet count, and BMI establishes a new standard for CSPH risk stratification, enhancing access to disease-modifying treatments for these patients.