Alcoholic liver disease
Alcohol is responsible for 3 million deaths every year (5.3% of global death).*11 Globally, over 50% of cirrhosis-related mortality is attributable to alcohol.7 Each time the liver filters alcohol, some of the liver cells die. Drinking heavily for many years can reduce its ability to regenerate with irreversible damage.

What is alcoholic liver disease?
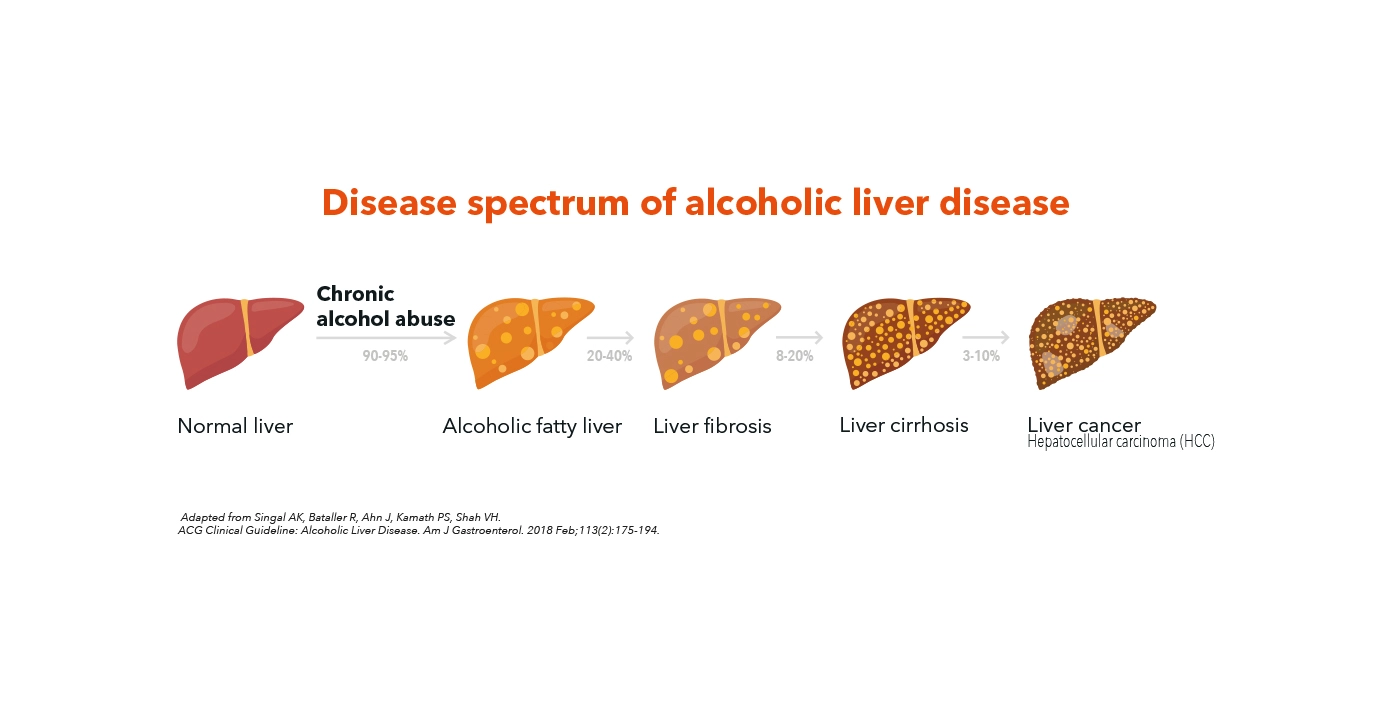
Alcoholic liver disease encompasses a wide clinical-histologic spectrum including alcoholic fatty liver, alcoholic hepatitis (AH), alcoholic steatohepatitis (ASH), and cirrhosis with its associated complications.
Diagnosis of alcoholic liver disease requires documentation of chronic heavy alcohol use and exclusion of other causes of liver disease.
Alcoholic steatohepatitis (fibrosis)
Alcoholic liver disease follows a well-recognized pattern of disease progression. It starts with alcoholic fatty liver, and some individuals might develop hepatic inflammation, ballooning and liver cell injury, which is histologically defined as alcoholic steatohepatitis (ASH), that will progress slowly to cirrhosis and associated complications such as hepatocellular carcinoma (HCC).
Alcoholic hepatitis (inflammation)
In addition to alcoholic steatohepatitis (ASH), individual might also present with Alcoholic hepatitis (AH) which is an acute hepatic inflammation associated with significant morbidity and mortality.
Who is at-risk of alcoholic liver disease?
Disease is caused by chronic consumption of alcohol exceeding a certain amount. Chronic alcohol consumption of 12-24 g per day has been demonstrated to significantly increase the risk of cirrhosis as compared to non-drinking.22
Why screening at-risk patients of alcoholic liver disease is important?
Most of patients are diagnosed at advanced stages and data on the prevalence and profile of patients with early disease are limited. As a result, identification of alcoholic liver disease in primary care settings at early stages is key to promote behavior, change and reverse the course of disease.
Damage to the liver caused by chronic liver diseases can often be reversed by early diagnosis and intervention.7
Our liver health solutions, FibroScan® and Scores by echosens allow a comprehensive management of liver health.
There is very good evidence for using transient elastography by FibroScan® for assessment of fibrosis in alcohol-related liver disease.
* Including deaths related to alcohol-associated diseases in different organs as well as injuries related to traffic accidents and violence.
References are available in our bibliography.